Venous Thrombosis Treatment
If venous thrombosis is suspected, it is a medical emergency and venous thrombosis treatment must be initiated immediately. In order to start venous thrombosis treatment quickly and adequately, further diagnostics are necessary. If acute venous thrombosis is suspected, we can perform duplex sonography at any time.

Recognize a venous thrombosis
Acute venous thrombosis is often noticeable by a feeling of tightness and one-sided leg swelling in the case of venous thrombosis of the leg or arm swelling in the case of venous thrombosis of the arm.
Venous thrombosis of the calf is the most common form, accompanied by a usually acute pain in the calf. The dull pain in the lower leg can therefore be the first sign of venous thrombosis. Typical triggers of venous thrombosis are any kind of immobilization: long distance flights, long train or car rides, hospitalization with bed confinement, etc. However, venous thrombosis can often occur without a clear trigger, “out of the blue” so to speak. Acute venous thrombosis of the arm often occurs after a blood sample has been taken or an indwelling venous cannula has been inserted: via an initially superficial venous thrombosis, the thrombotic clot material grows into the deep venous system and causes acute venous thrombosis here. In order to detect a venous thrombosis, an ultrasound examination is necessary. It can be used to reliably detect or rule out venous thrombosis.
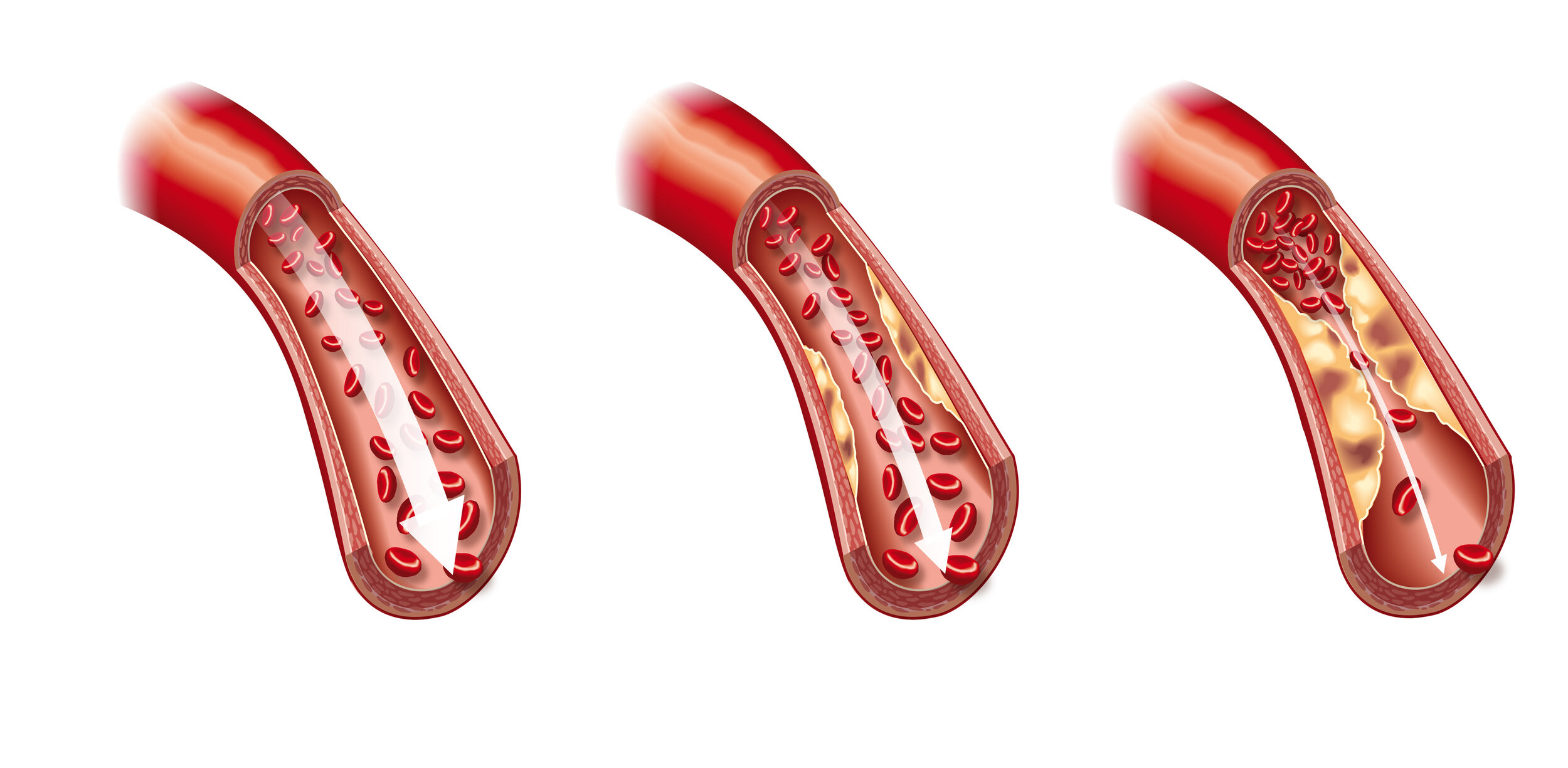
Venous thrombosis treatment must be initiated immediately if venous thrombosis is detected. Venous thrombosis treatment is intended to prevent further growth of the venous thrombosis. Another danger is concomitant pulmonary artery embolism. This arises from acute thrombosis in the deep venous system, usually venous thrombosis of the leg, due to thrombotic material in the deep conducting veins, which travels back to the heart via the venous system with the blood flow and then becomes entrapped in the lungs. Venous thrombosis treatment is started with blood thinning. Here, either heparin or an oral blood thinner as a tablet is given. This is accompanied by the fitting of an appropriate compression stocking or, in the case of pronounced leg swelling, the leg is first bandaged with a compression bandage.
A frequent cause for the development of acute venous thrombosis is varicose vein disease of the superficial skin veins. Initially, superficial venous thrombosis also occurs here, which then passes into the deep venous system via connecting veins / so-called bridging veins and can cause acute venous thrombosis. If varicose veins have already caused superficial phlebitis, varicose vein treatment is recommended. In contrast to the almost obvious superficial venous thrombosis, acute venous thrombosis of the deep veins can only be recognized clinically in a more unspecific way: e.g. by a difference in circumference of the affected extremity or by leg swelling. However, there is also an increased risk of thrombosis after any vein intervention, be it surgical varicose vein removal or spider vein treatment. Therefore, in the follow-up treatment of patients who have undergone vein surgery or other manipulations of the superficial leg veins, in addition to regular checks, it is necessary to wear a compression stocking as a prophylaxis to prevent the development of venous thrombosis. Under certain circumstances, drug treatment with heparin may also be necessary for the prophylaxis or treatment of venous thrombosis.
Lymphedema should also be considered if leg swelling is present. In this case, the swelling is predominantly in the forefoot. Lymphedema treatment is primarily based on physical treatment procedures. In addition to lymphatic drainage, this includes the fitting of a special compression stocking, similar to the treatment of venous thrombosis. Drug therapy with a blood thinner is not necessary here.
Arteriosclerosis treatment, on the other hand, also often involves the use of blood thinning drugs. Therefore, if acute venous thrombosis is present at the same time as PAOD, venous thrombosis treatment must be adapted accordingly and determined on an individual basis.
In summary, if there are signs of venous thrombosis, a medical presentation must be made immediately to confirm the suspicion and venous thrombosis treatment can be initiated promptly.