What can you do yourself in addition to the therapy of PAOD?
In addition to stopping smoking, a healthy diet and regular exercise are also important in the treatment of arteriosclerosis. Structured walking training can also improve the circulatory disorder and lead to a reduction in symptoms. Collateral pathways, so-called collaterals, are thereby promoted and developed.
The treatment of PAOD is based on stages I to IV. In the initial stage, the blood flow is still sufficient even under physical strain, so that there are still no complaints (stage I). If the vasoconstriction increases, there is pain when walking, i.e. the so-called “shop window disease”, which forces the patient to stop walking. After a short pause, walking can be continued as the muscles are supplied with oxygen again (stage II). If pain occurs at rest, especially when lying down, there is a critical circulatory disorder (stage III). In the final stage of PAOD, damaged or dead tissue occurs, and open wounds and ulcers may form, especially on the toes (stage IV). Amputation may become necessary.
Why is PAOD dangerous and should be treated and diagnosed early?
For a long time, the disease goes unnoticed, as it does not cause any symptoms in the early stages. If symptoms do occur, they are often misinterpreted as orthopedic complaints. However, arteriosclerosis not only leads to circulatory disorders in the arteries of the legs, but also in the arteries of the heart and brain. Patients with PAOD have a 3-fold increased risk of stroke or heart attack.
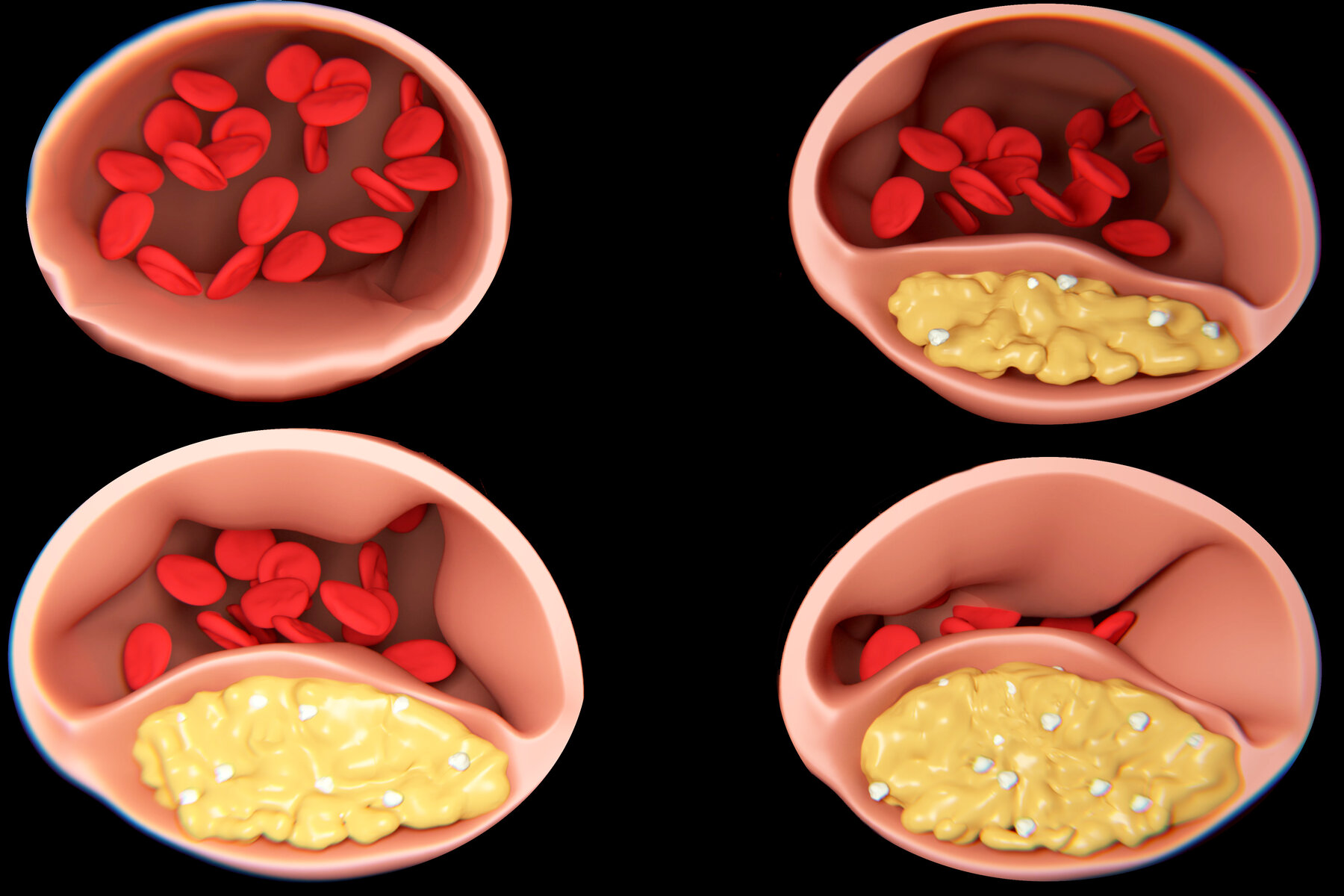
The vascular deposits, also called plaques, not only lead to vasoconstriction, but can also cause arterial occlusion. This acutely interrupts the oxygen supply to the area supplied by the vessel. Acute pain and pallor of the skin as a symptom may require immediate diagnosis and therapy. Otherwise, tissue death, possibly even amputation, may occur.
How is the diagnosis of PAOD made?
In addition to a detailed medical history and physical examination, the basic examination includes Doppler pressure measurement as a quick, painless and informative method. The blood pressure at the upper arms and ankles is measured by means of a Doppler probe. The so-called ankle-arm index is determined.
Pulse oscillography and treadmill ergometry are also part of the diagnosis of PAOD, but above all color-coded duplex sonography, vascular ultrasound. Ultrasound is a painless, harmless and very informative method for PAOD diagnostics. The vascular system with its changes can be displayed on a monitor. The blood flow in the arteries can be shown by color.
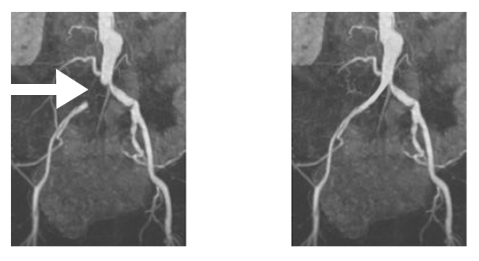
Complementary methods for imaging vessels are computed tomography (CT), i.e. CT angiography, or magnetic resonance (MR) angiography. These are also particularly suitable for the diagnosis of the abdominal and pelvic vessels, which are sometimes difficult to visualize in vascular ultrasound, e.g. in the case of intestinal gas overgrowth or obesity.
The most accurate method for visualizing vascular stenoses and occlusions is angiography with X-ray contrast medium, so-called digital subtraction angiography. In this procedure, the artery in the groin is punctured after local anesthesia. The contrast medium is introduced into the vascular system via a thin plastic tube and the vessels can be visualized using X-rays. Due to the use of modern equipment, the radiation exposure is low.
The therapy of PAOD is usually carried out according to the stages already described. The goal of treatment is to lower the risk of cardiovascular disease by treating the risk factors. This can reduce the risk of stroke, heart attack and sudden cardiac death. It also aims to prevent the progression of PAOD and improve quality of life (by, for example, relieving symptoms).
In stage I, the patient is still symptom-free. Treatment of the risk factors (change in lifestyle and drug treatment) is the focus here and represents the basis of PAOD therapy for all stages. If pain on exertion occurs (stage II), the pain-free walking distance can be extended by consistent walking training. It makes sense to participate in vascular sports groups.
If this does not improve the quality of life, the walking distance is less than 200 m or the PAOD causes great pain, catheter therapy should be performed. In this process, the physician attempts to dilate vascular constrictions (so-called balloon dilatation), and in the case of more complicated or longer constrictions, a stent (vascular support) is inserted in the process. Vascular occlusions can also be removed and blood flow restored with new therapies for PAOD. Catheter treatment of PAOD is performed without general anesthesia. Local anesthesia is used only in the groin area. A short hospital stay is usually required.